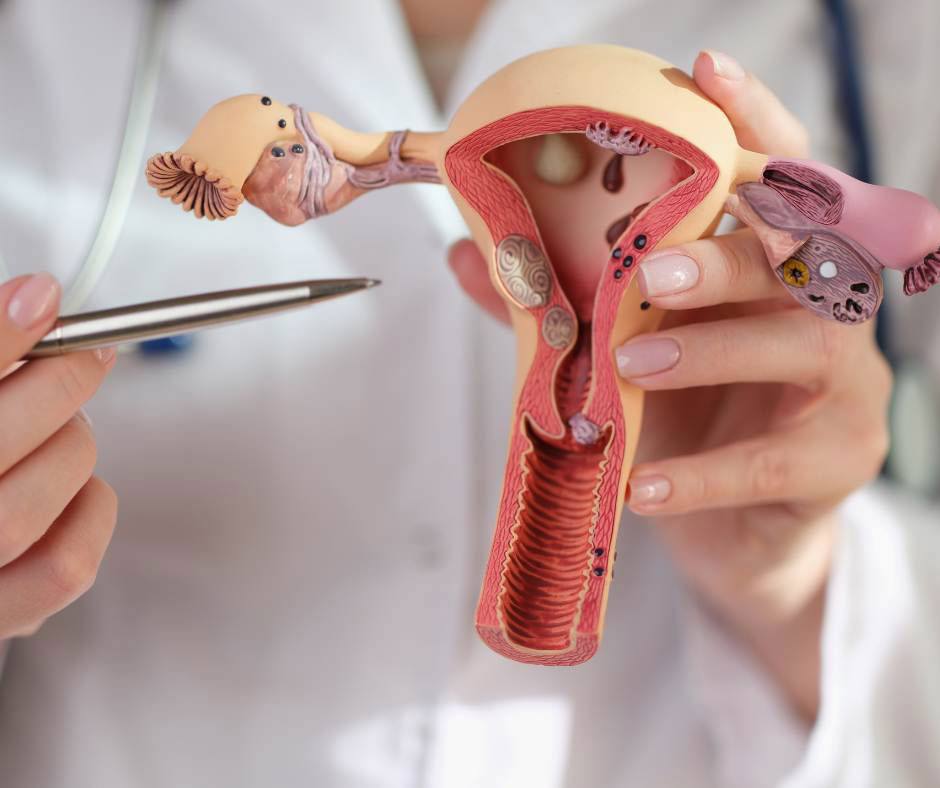
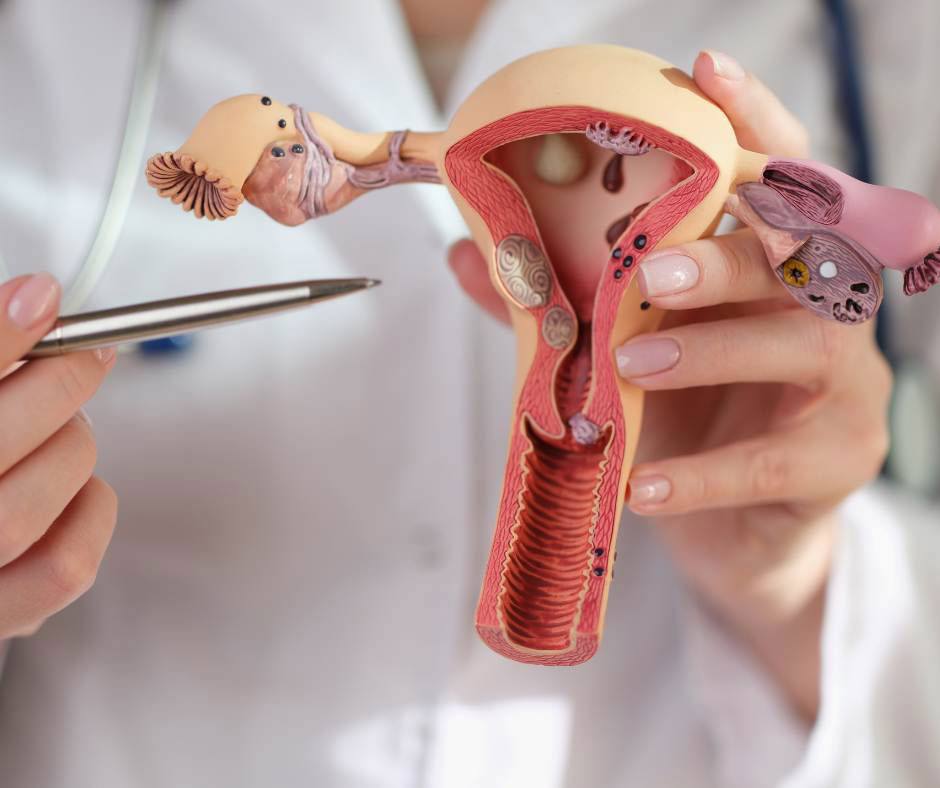
Uterine Cancer:
The uterus is the warm place that holds the fetus until birth. Like other female reproductive organs, the uterus undergoes many hormonal changes during the menstrual cycle and may also undergo various pathological changes. The most concerning for women is uterine cancer, which often occurs during menopause (the period following the cessation of menstruation). Most affected women may have been exposed to risk factors during their lives or have a genetic predisposition to uterine cancer.
Uterine Cancer occurs, like other types of cancers, as a result of loss of control over uterine cells. These cells begin to divide rapidly and uncontrollably, producing tissues that form a tumor. The growth of these cells can occur in the endometrial lining of the uterus or in the myometrium or the supporting tissues of the uterus. Based on this, uterine cancer is divided into two main types: endometrial cancer and uterine sarcoma.
Who is at risk for uterine cancer:
In fact, all women can develop uterine cancer, but it becomes more common with advancing age (over 50 years old). Women approaching menopause or during menopause are most at risk of developing uterine cancer. Other risk factors include:
1- Obesity or overweight (unhealthy high amounts of fat).
2- Taking female hormones such as estrogen during menopause (as hormone replacement therapy without taking other hormones such as progesterone).
3- Difficulty getting pregnant.
4- Taking tamoxifen, a drug used to treat certain types of breast cancer.
5- Women with a family history of colon, uterine, or ovarian cancer.
- It is important to screen and detect uterine cancer early, as early detection leads to more effective treatment. Having these risk factors doesn't necessarily mean you will get uterine cancer, but it's crucial to talk to your doctor for various screenings and routine check-ups.
Signs and symptoms of uterine cancer include:
1- Abnormal vaginal discharge.
2- Unusual vaginal bleeding: excessively heavy or occurring outside of menstrual cycles or post-menopausal bleeding, which might also be prolonged.
3- Pelvic pain or pressure, or difficulty urinating.
4- Pain during intercourse.
Be attentive to your body and promptly consult a doctor if you notice any changes or any of the above symptoms persist for two weeks or more. These symptoms may not definitively indicate uterine cancer, so it's essential to see a doctor to rule out other potential causes.
Can you prevent uterine cancer:
There's no foolproof way to prevent uterine cancer, but you can take measures to reduce your risk:
1- Use birth control pills.
2- Maintain good health and weight, and exercise regularly.
3- Do not neglect progesterone hormone (when taking estrogen hormone replacement therapy after menopause), as it's used to treat postmenopausal
symptoms like hot flashes. - Uterine Cancer Diagnosis:
Women without symptoms or a family history of uterine cancer aren't typically recommended for routine screenings. A gynecologist performs various tests to determine if you have uterine cancer and may refer you to a gynecologic oncologist. Your doctor will need your medical history, assess your risk factors, and conduct a thorough physical exam, including pelvic examination. Diagnostic tests may include:
*- Transvaginal ultrasound: Utilizes a probe moved over your lower abdomen to create images on a screen, helping detect masses or tumors.
*- Endometrial biopsy: Often used to diagnose uterine lining cancer, involving the insertion of a thin tube to suction out a small amount of tissue, usually performed in a doctor's office.
*- Hysteroscopy: A small telescope is inserted into the uterus to obtain a clearer view of the interior, with or without tissue sampling, sometimes using local anesthesia.
*- Dilation and curettage (D&C): If biopsy samples are inadequate or if cancer is suspected but not confirmed, this procedure involves scraping tissue from inside the uterus, typically under general anesthesia.
If your doctor suspects advanced uterine cancer, additional diagnostic tests may be necessary to rule out spread to other tissues, such as CT scans, MRI, PET scans, cystoscopy, and comprehensive blood tests. Consult a gynecologic oncologist for further details about your case.
Treatment:
Surgical treatment is common and may involve procedures such as total hysterectomy, including removal of the uterus and cervix either vaginally or through an abdominal incision, or via minimally invasive methods like laparoscopy. Additional surgeries may include removal of the ovaries and fallopian tubes or radical hysterectomy, which removes the uterus, cervix, part of the vagina, and possibly other nearby tissues.
After surgery, the doctor may use hormonal or radiation therapy to target remaining cancer cells and reduce the risk of recurrence.
Radiation therapy utilizes high-energy x-rays or other types of radiation to kill cancer cells. It can be external, where the machine is outside the patient's body, or internal, where radioactive material is placed directly into the uterus.
Chemotherapy involves using specific drugs to stop cancer cell growth or division, administered orally, intravenously (affecting wider areas of the body, leading to more severe side effects), or locally within the body cavity or affected area.
Hormone therapy aims to stop hormone production and thus inhibit cancer cell growth.
Since these treatments can have potent effects not limited to cancer cells, they may cause various side effects, such as anemia, appetite loss, bruising, digestive issues, confusion, fatigue, swelling, fertility issues in women, memory/concentration problems, nausea, skin/nail changes, sleep problems, and urinary tract issues.
Side effects can vary widely among individuals receiving the same treatment.
Ultimately, upon uterine cancer diagnosis, prompt treatment initiation is crucial for effective management. Seek emotional and social support from your surroundings and choose the right doctor for optimal care.